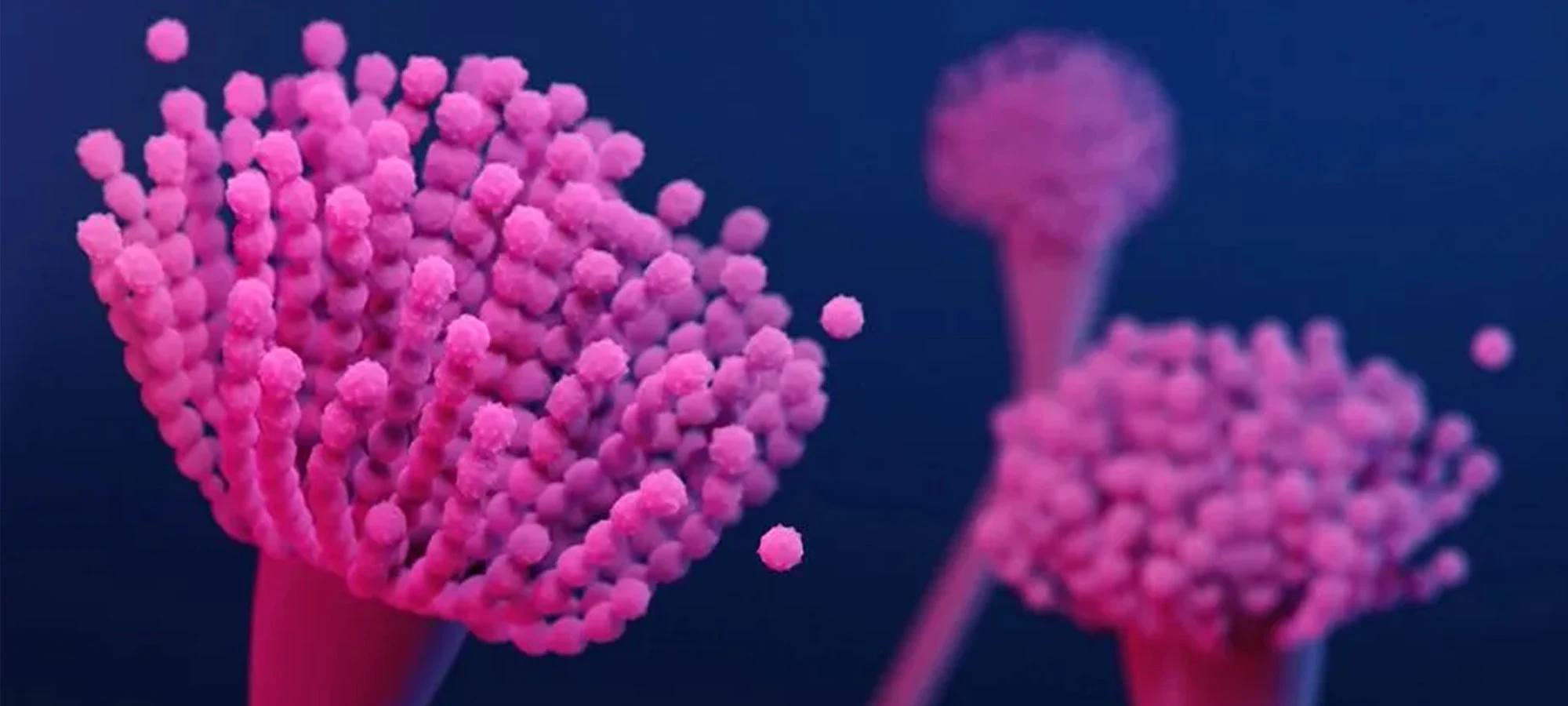
The human gut is a complex ecosystem, and sometimes, unwelcome residents can disrupt its delicate balance, leading to significant health concerns. One such microscopic intruder is Helicobacter pylori (H. pylori), a bacterium that colonises the stomach lining of roughly half the world's population. While many infected individuals remain asymptomatic, for others, H. pylori can be a silent instigator of chronic gastritis, peptic ulcers, and, in some cases, increase the risk of developing stomach cancer.
Given its potential for harm, accurate and timely detection of H. pylori is paramount. For years, diagnostic approaches varied, often involving invasive procedures like endoscopy with biopsy, or less direct methods. However, a significant advancement in non-invasive diagnostics has been the H. pylori Stool Antigen Test (HpSA). This test has fundamentally changed how we approach the diagnosis and management of this common yet consequential infection.
What makes the H. pylori Stool Antigen Test a diagnostic cornerstone?
The beauty of the HpSA test lies in its directness and simplicity. It works by detecting specific antigens - proteins produced by the H. pylori bacterium - directly in a patient's stool sample. The presence of these antigens is a clear indicator of an active infection. This is a crucial distinction, as some other tests, like certain blood antibody tests, can only indicate past exposure to the bacteria rather than a current, active colonisation requiring treatment.
The non-invasive nature of the stool antigen test is perhaps its most celebrated advantage. It eliminates the discomfort, risks, and higher costs associated with endoscopic procedures, making it a far more patient-friendly option, especially for initial diagnosis. This ease of sample collection also makes it highly suitable for diverse patient populations, including children and individuals for whom more invasive tests might be contraindicated or challenging.
Beyond initial diagnosis, the H. pylori Stool Antigen Test plays a vital role in confirming eradication after a course of treatment. It's not enough to simply complete the antibiotic regimen; verifying that the bacteria have been successfully eliminated is essential to prevent recurrence of symptoms and long-term complications. The stool antigen test, performed a few weeks after therapy completion (and ensuring the patient has been off certain medications like proton pump inhibitors and antibiotics for an appropriate period), provides reliable confirmation of treatment success.
Furthermore, in an era focused on antimicrobial stewardship, accurate diagnosis prevents the unnecessary use of antibiotics. The HpSA test helps clinicians make informed decisions, targeting therapy specifically to those who will benefit, thereby reducing the risk of antibiotic resistance and side effects.
While the H. pylori Stool Antigen Test is highly accurate and reliable, like any diagnostic tool, its results are best interpreted within the full clinical picture. It's important for patients to follow pre-test instructions carefully, particularly regarding the temporary discontinuation of medications like proton pump inhibitors (PPIs) and antibiotics, which can interfere with the test and potentially lead to false-negative results. Clinicians will consider symptoms, medical history, and other relevant factors alongside the test outcome.
The H. pylori Stool Antigen Test represents a significant step forward in managing a prevalent and potentially serious infection. Its ability to offer a non-invasive, accurate assessment of active infection and treatment efficacy makes it an invaluable asset in safeguarding gastric health. For individuals experiencing persistent upper abdominal discomfort, or for whom H. pylori infection is suspected, this simple test can be the key to uncovering the culprit and paving the way for effective relief and long-term well-being.