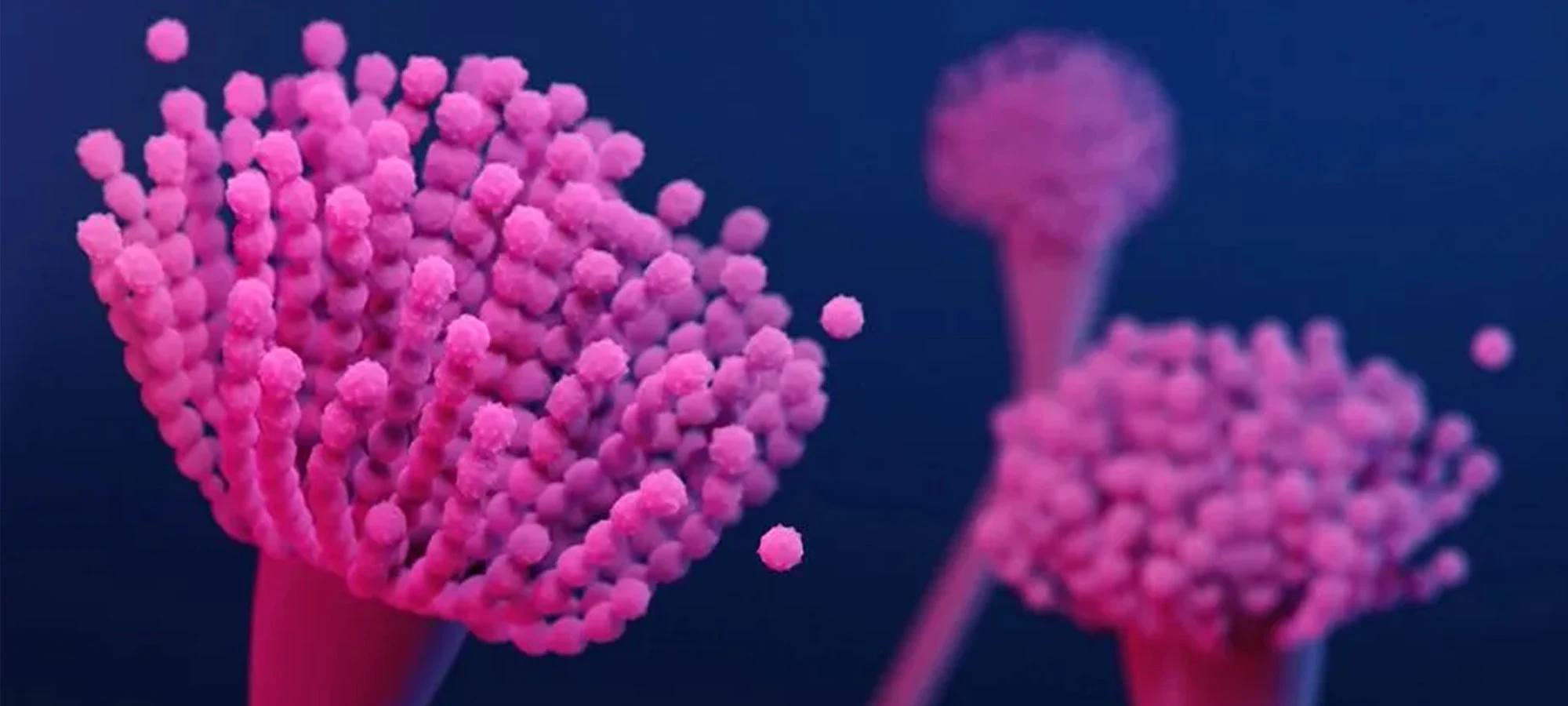
In the intricate world of medical diagnostics, some challenges loom larger than others. Among these is the timely detection of Invasive Aspergillosis (IA), a severe and often life-threatening fungal infection caused by species of Aspergillus. While Aspergillus moulds are ubiquitous in our environment and generally harmless to healthy individuals, they can become formidable pathogens in those with compromised immune systems - patients undergoing chemotherapy, organ or stem cell transplant recipients, or individuals on long-term corticosteroids.
The insidious nature of IA lies in its often non-specific clinical presentation, mimicking other respiratory conditions. Traditional diagnostic methods, such as culture, can be slow and may lack sensitivity, leading to critical delays in initiating appropriate antifungal therapy. This diagnostic gap is precisely where the Galactomannan (GM) Aspergillus Antigen test emerges as a pivotal tool.
Galactomannan is a polysaccharide, a key component of the Aspergillus cell wall, which is released into the bloodstream and other body fluids like bronchoalveolar lavage (BAL) fluid during active, invasive fungal growth. The GM test is designed to detect this specific antigen, providing a valuable biomarker for infection.
Why is this test so important?
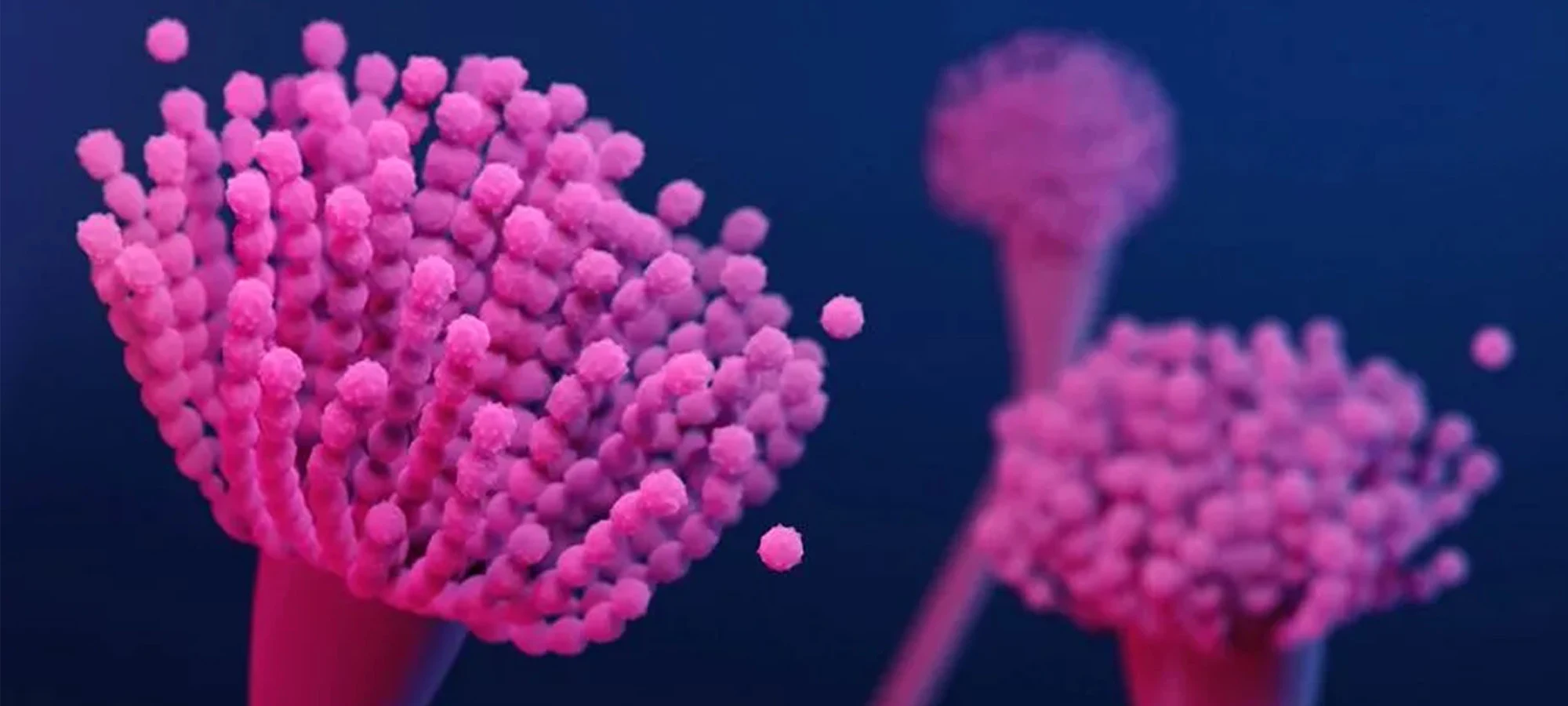
Its primary advantage lies in its ability to detect the presence of Aspergillus often before clinical symptoms become pronounced or before other diagnostic methods yield positive results. This early warning is crucial. In the context of IA, where the infection can progress rapidly, early initiation of targeted antifungal treatment significantly improves patient outcomes and can be life-saving.
Furthermore, the Galactomannan test offers a less invasive route to diagnosis compared to procedures like lung biopsies, which carry inherent risks, especially for critically ill patients. Serial GM testing can also be invaluable in monitoring the response to antifungal therapy and detecting early signs of relapse, allowing clinicians to adjust treatment strategies proactively. It aids clinicians in differentiating IA from other febrile illnesses in high-risk patients, guiding targeted treatment decisions rather than empirical, broad-spectrum approaches.
The utility of GM testing is most pronounced in specific patient populations, particularly those with prolonged neutropenia, haematological malignancies, recipients of allogeneic hematopoietic stem cell or solid organ transplants, and patients on high-dose corticosteroids or other potent immunosuppressive agents. For these vulnerable individuals, proactive screening or prompt testing at the first sign of potential infection can make all the difference.
However, it's crucial to understand that the Galactomannan test is not a standalone diagnostic. Results must always be interpreted within the broader clinical context, considering patient risk factors, symptoms, and other radiological or microbiological findings. Factors such as certain medications (e.g., some beta-lactam antibiotics that cross-react, or contamination from food sources in rare cases) can occasionally lead to false-positive results, while the sensitivity can vary depending on the patient's immune status, the burden of fungal disease, and the site of infection. Therefore, clinical acumen remains paramount.